This article identifies some of the issues arising for care homes in respect to end of life care and suggests some remedies.
It is recognised that very often families do not want to talk about end of life care and the staff may feel inadequately equipped to broach such sensitive conversations especially in the face of strong emotions such as guilt, denial, anxiety, difficulty letting go etc. There are issues around individual preferences and whether these have been identified and recorded. There may be no next of kin, or no living relatives, the client has advanced dementia or incapacity so the Office of the Public Guardian will be involved. Sometimes there are disputes within the family and a best interest decision may be needed with GP input. All these difficult scenarios can be alleviated by the right training and skill base within the staff team. Staff who have been trained to be alert for signs of impending death and in skilful communication are essential. They can make the difference between a ‘good death’ or a poor one that leaves family and staff distressed and exposes the Care Home to complaints, loss of reputation or worse still, litigation.
Definition of end of life care
– People are ‘approaching the end of life’ when they are likely to die within the next 12 months. This includes patients whose death is imminent (expected within a few hours or days) and those with: a) advanced, progressive, incurable conditions; b) general frailty and co-existing conditions that mean they are expected to die within 12 months; c) existing conditions if they are at risk of dying from a sudden acute crisis in their condition; d) life-threatening acute conditions caused by sudden catastrophic events
Dying without dignity
Poor communication and not recognising that people are dying were key themes identified by a Parliamentary and Health Service Ombudsman’s investigation into complaints about end of life care, ‘Dying without dignity’. Correctly recognising that a person is in the last days of life may allow opportunities for shared decision‑making and prevent unnecessary interventions. Good communication of a dying person’s prognosis improves their end of life care and the bereavement experience of those important to them. It can help to ensure that the dying person’s expressed wishes are considered and to avoid misunderstandings and unnecessary distress.
“The Ombudsman Committee considers that all clinicians and providers should be aware of the Five Priorities of Care that were outlined by the Leadership Alliance for the Care of Dying People in its report One Chance to Get it Right in June 2014:
- The possibility that a person may die within the next few days or hours is recognised and communicated clearly, decisions are made and actions taken in accordance with the person’s needs and wishes, and these are regularly reviewed and decisions revised
- Sensitive communication takes place between staff and the dying person, and those identified as important to
- The dying person, and those identified as important to them, are involved in decisions about treatment and care to the extent that the dying person
- The needs of families and others identified as important to the dying person are actively explored, respected and met as far as
- An individual plan of care, which includes food and drink, symptom control and psychological, social and spiritual support, is agreed, co-ordinated and delivered with ”
https://www.ombudsman.org.uk/publications/dying-without-dignity/introduction
NICE guideline (2015)
This guideline aims to improve end of life care for people in their last days of life by communicating respectfully and involving them, and the people important to them, in decisions and by maintaining their comfort and dignity. The guideline covers how to manage common symptoms without causing unacceptable side effects and maintain hydration in the last days of life.
The guideline is intended for all healthcare professionals and other care providers.
It provides recommendations to help recognise when a person is entering the last days of life or may have stabilised or be improving even temporarily; to communicate and share decisions respectfully with the dying person and people important to them; and to manage hydration and commonly experienced symptoms to maintain the person’s comfort and dignity without causing unacceptable side effects.
https://www.nice.org.uk/guidance/ng31
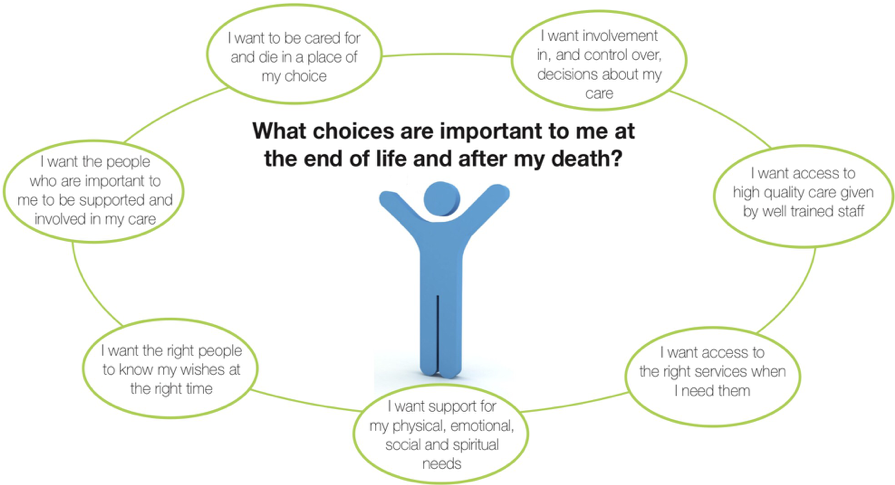
The National Council for Palliative Care promotes the need for choice at the end of life
“We believe that asking everyone who is approaching the end of their lives a single question
“what’s important to you?” can open the gateway to conversations that ensure people have choices and care that are focused around their needs.”
The NCPC suggests these three elements are crucial:
- Staff training particularly in respect of two important areas:-
- Identifying when a client is approaching
- Building the skills required for communicating openly and frankly with relatives or
- Named responsible clinicians, in many cases this will be the The most important thing is that the Care Home has alerted the GP and established this arrangement and that this is recorded in the Care Plan
- Identified care coordinators within the Care Home. See below for specific training for http://www.ncpc.org.uk/sites/default/files/ CHOICE%20REVIEW_EXECUTIVE%20SUMMARY_WEB.pdf
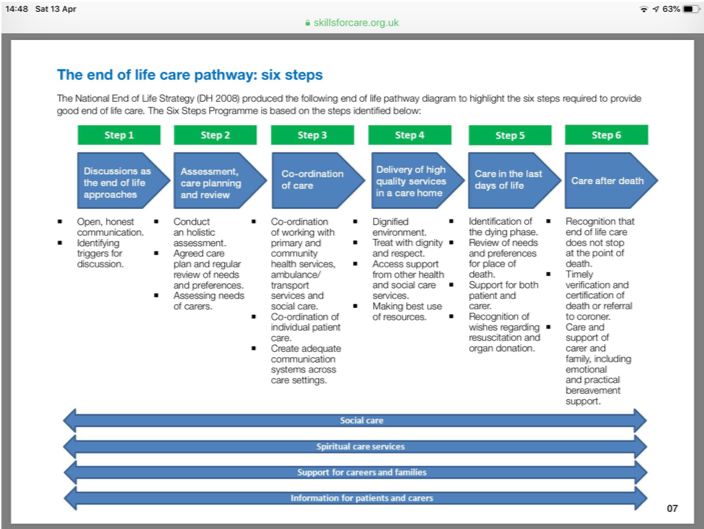
Training resources. ‘Six Steps Programme’
The Six Steps Organisational Programme is free and specifically aimed at care homes. Participants are required to develop a portfolio of evidence to demonstrate that they have met the outcomes of the programme. This portfolio is divided into FIVE SECTIONS that align to the five key questions that are asked by the Care Quality Commission (CQC) during inspections. KLOE R3 specifically relates to end of life care, however, good end of life care spans across many of the KLOEs. The portfolio remains in the care home and can be shared with commissioners, Local Authority monitors and CQC.
http://eolp.co.uk/SIXSTEPS/download/2985/
Below, a graphic produced by Skills for Care shows the components of the Six Steps approach to improving end of life care. (There is a specific module available on end of life care for clients with Dementia).
An example of the content of training for end of life care co-ordinators.
Six Steps training for care coordination ……
Time: Half day
Aim: A system is in place to ensure coordination of care takes place
Objectives: By the end of the session the domiciliary care worker will be able to:
- Identify the value of good communication systems in end of life care
- Recognise the importance of sharing information with the wider multidisciplinary team
- Recognise the key features and values of the role of a Key Worker / care coordinator
- Be aware of aspects of anticipatory needs at the end of life
- Identify necessary and unnecessary admissions to acute care
A case study of a Care Home in Norwich.
Ivy Court deputy manager Vanessa Soares explained: “It is our aim to give the best care we can to our residents and the Six Steps programme is proven to lead to better end of life care by increasing our knowledge and awareness of the issues. Evidence of our commitment to the programme will be kept in a portfolio that everyone can reference.”
https://chmonline.co.uk/six-steps-to-the-best-end-of-life-care-at-ivy-court/
A highly rated Book with a practical, down to earth approach is available here. https://www.scie-socialcareonline.org.uk/a-practical-guide-to-end-of-life-care/r/ a11G000000CTEgdIAH
A useful training video addressing the issues around lack of advanced care decisions https://learning.elucidat.com/course/5b5f314583a6e-5bacd8278d3e2